In the 2018 Quality Payment Program proposed rule, published in the Federal Register on June 30, the Centers for Medicare & Medicaid Services (CMS) estimates that approximately 572,000 clinicians will be required to submit data under the Merit-based Incentive Payment System (MIPS) in the second performance year. CMS estimates that between 180,000 and 245,000 of […]
AAPC Knowledge Center
Laureen shows you her proprietary “Bubbling and Highlighting Technique”
Download your Free copy of my "Medical Coding From Home Ebook" at the top right corner of this page 2018 CPC Practice Exam Answer Key 150 Questions With Full Rationale (HCPCS, ICD-9-CM, ICD-10, CPT Codes) Click here for more sample CPC practice exam questions with Full Rationale Answers Click here for more sample CPC practice exam questions and answers with full rationaleTag Archives: Impact
Upcoming IMPACT Act Special Open Door Forum
E/M new or established rule and tax ID impact?
By CPT definition, a new patient is one who has not received any professional services from the physician, or another physician of the same specialty who belongs to the same group practice, within the past three years.
CMS guidance states, For purposes of billing for E/M [evaluation and management] services, patients are identified as either new or established, depending on previous encounters with the provider. A new patient is defined as an individual who has not received any professional services from the physician/non-physician practitioner (NPP) or another physician of the same specialty who belongs to the same group practice within the previous three years.
IMPACT Act, VBP, care coordination, and the SNF landscape
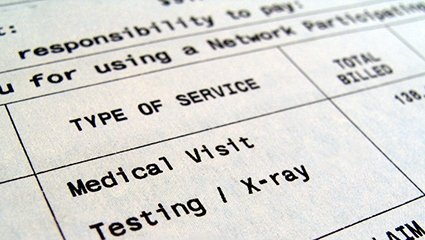
Assessing the Impact of High Deductible Health Plans on Radiology Practices
Before the days of managed care, insurance plans were “indemnity coverage” that reimbursed patients for their out-of-pocket costs. Physicians billed the patients and got paid when the patients felt like making payment, usually only after the insurance company had reimbursed them. Often, the insurance money went elsewhere in the patient’s budget and the physician waited for payment. The not-so-good old days! With the advent of managed care contracting where physicians were paid directly by the insurance company, patient balance collections mostly disappeared. Today the pendulum is swinging back in the opposite direction, requiring practices to once again face the necessity to collect significant balances from patients.
Hospital Industry Warns Trump, Congress About ACA Repeal Impact
The hospital industry wants President-elect Donald Trump and congressional leaders to preserve coverage gains when repealing the Affordable Care Act (ACA) and, if not, they want legislators to repeal funding reductions for hospital services in the ACA. In a letter to the incoming administration and another to Congress, the American Hospital Association (AHA) and Federation of American […]
AAPC Blog