MOON requirement delayed in IPPS final rule: What next?
Hospitals got a last-minute reprieve from the Medicare Outpatient Observation Notice (MOON) notification requirement, which was set to go into effect August 6. Citing the need for additional time to revise the standardized notification form that hospitals will need to use to notify patients about the financial implications of being assigned to observation services, CMS moved back the start date for the requirement in the 2017 IPPS final rule to ‘no later than 90 days,’ after the final version of the form is approved (www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/AcuteInpatientPPS/FY2017-IPPS-Final-Rule-Home-Page.html).
CMS released the new draft of the form (www.cms.gov/Regulations-and-Guidance/Legislation/PaperworkReductionActof1995/PRA-Listing-Items/CMS-10611.html?DLPage=1&DLEntries=10&DLFilter=10611&DLSort=1&DLSortDir=descending) August 1 and accepted public comments for 30 days. The MOON notification form is intended to be used to help hospitals comply with the Notice of Observation Treatment and Implication for Care Eligibility (NOTICE) Act. The Act requires hospitals to provide a verbal and written notice of outpatient status to any patient in observation who has been in the hospital for more than 24 hours, stipulating that hospitals must inform patients within 36 hours from the start of the service about their status. However, without a final version of the form ready for use, it would appear that hospitals cannot comply with the NOTICE Act at this time.
‘Hospitals should review the IPPS final rule that contains significant clarification on things like when and how the notice is delivered and finalize their own policies for delivering the notice pending the final version of the MOON being available,’ says Kimberly Anderwood Hoy Baker, JD, CPC, director of Medicare and compliance for HCPro in Middleton, Massachusetts.
CMS stated in the 2017 IPPS final rule:
We expect the final [Paperwork Reduction Act] PRA approval of the MOON around the time the implementing regulations are effective. Therefore, the implementation period for hospitals and CAHs will begin sometime after the effective date of this final rule and will be announced on the CMS Beneficiary Notices Initiative Website at: www.cms.gov/Medicare/Medicare-General-information/Bni/index.html and in an HPMS memorandum to MA plans. During this implementation period, hospitals and CAHs will have time to prepare for implementation, consistent with past implementation practices for beneficiary notices. Hospitals and CAHs will be required to deliver the MOON to applicable patients who begin receiving observation services as outpatients on or after the notice implementation date.
‘Hospitals should watch the Beneficiary Notice Initiative page, where CMS said they would announce implementation information, for more information on the finalization of the MOON and implementation time frames,’ says Baker.
Hospitals will likely not be required to provide the MOON notification form to patients until 90 days after PRA approval, which could mean compliance with the MOON and NOTICE Act is at least 120 days out from the final rule release date given that there is also a 30-day comment period on the revised form, according to Baker.
‘When the final version of the notice form is ready for use, hospitals should use the 90-day implementation period to develop a mechanism for the form to be in their EHR with a trigger to print the notice when the patient is registered as or has a status change to observation. This will allow for the form to be delivered by the designated individual to the patient immediately rather than attempting to do it at discharge,’ says Rose T. Dunn, MBA, RHIA, CPA, FACHE, chief operating officer for First Class Solutions, Inc.
The message should be delivered by hospital staff who are well versed in the purpose of the notice and how patient status may financially impact the patient. Dunn recommends that hospitals choose patient access staff, financial counselors, or utilization review/case management staff to deliver the MOON rather than patient care staff.
The role of HIM in MOON compliance
While many facilities plan to task departments outside of HIM with delivering the verbal and written notice to observation patients, that does not mean there isn’t a seat at the table for HIM when it comes to operationalizing this regulation.
At Via Christi Health in Wichita, Kansas, Sam Antonios, MD, FACP, FHM, CCDS, medical director of medical information and ICD-10 physician advisor, and his colleagues are working to ensure they understand the nuances of the MOON.
Antonios’ facility is currently building a daily report to help track patients who have been in observation 24 hours.
The report will help the facility ensure compliance with the NOTICE Act and MOON, but this may be a challenge for facilities that do not have the capability to create such a document in their electronic systems. But even with the right systems and alerts in place, relying on just one report may present challenges. ‘For example, you may have patients who don’t have the right trigger from the initiation of observation services,’ Antonios says. Remember, the MOON must be delivered 24?36 hours after the initiation of observation services, which is not always the time when the patient entered the hospital, especially for those in the emergency department, he says.
In general, HIM should aid in the creation of reports listing any admission for Medicare beneficiaries in observation. Records for patients who have been in observation for more than 24 hours should be flagged when the report is run, which should ideally be done twice daily and be sent to the team tasked with delivering the MOON, Antonios says.
HIM must play a role in deciding what to do with the MOON when it is completed and how to track verbal notification of observation status, Antonios says. Should HIM scan the MOON forms immediately for inclusion in the patient’s medical record, or should scanning be completed at the end of the patient’s hospital stay? Deciding which option is best may depend on the needs of your facility and staffing patterns.
‘HIM professionals should ensure that the form is properly signed and scanned into the appropriate section of the medical record where it can be consistently found during an audit,’ says Edward Hu, MD, CHCQM-PHYADV, system executive director of physician advisor services at UNC Health Care system in Chapel Hill, North Carolina, and president of the American College of Physician Advisors. In addition, HIM will also play a role in ensuring the CMS-approved MOON is given to observation patients, Hu says.
In an era when hospitals are increasingly using electronic methods of documentation and communication, it may be tempting to create an electronic version of the MOON for patients to read and sign. However, Hu notes that if this practice is implemented the patient must still receive a paper copy of the form. ‘Hospitals must provide a signed paper copy of the MOON to the beneficiary, even if he or she reviews and signs on an electronic pad,’ he says. ‘The hospital must provide the MOON on paper for the beneficiary’s review if the beneficiary asks to review a paper version.’
Tracking and delivering the MOON is one hurdle to overcome, but so too is ensuring that patients understand the information presented to them. Language barriers can present a challenge when delivering the MOON. While it may be relatively easy to obtain a copy of the notice for patients who speak more common languages like Spanish, it is a bit more difficult at Antonios’ facility where patients speak a variety of languages that the form is not available in. In turn, staff may have a difficult time verbally notifying patients of observation status during off hours when a translator is unavailable, he says.
Hu notes that HIM can play a role in ensuring the Spanish-language version of the MOON is made available to patients and staff when it is approved by CMS. ‘Hospitals also have an obligation to provide the information on the MOON in a language and manner that the patient understands. Although this does not mean the MOON must be translated into every language, it does mean that the hospital has an obligation to ensure understanding by beneficiaries with limited English proficiency,’ he says.
The ups and downs of MOON
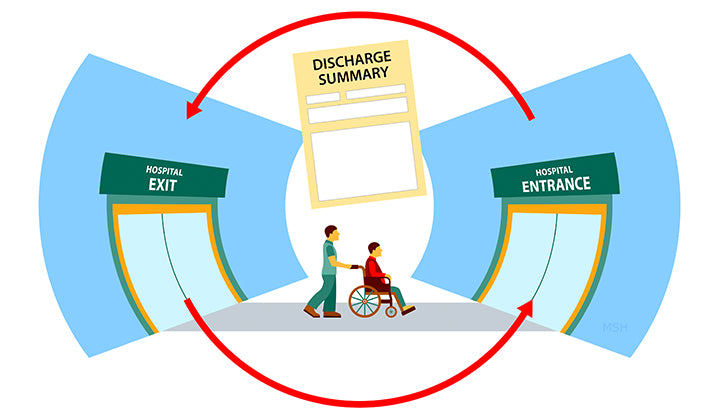
Complying with the NOTICE Act and operationalizing MOON has presented a significant challenge for healthcare organizations. Some are unsure of how to deliver the form and little is known about the impact it will have on patient relations and hospital staffing.
The verbal and written notice to observation patients should be given between 24 and 36 hours of the patient being placed in this status, which has many wondering whether they should actually wait 24 hours to deliver the notice since it can be challenging to ensure the notice is given before the 36-hour mark, says Antonios. ‘It leaves you with an open window of only 12 hours of actually being able to deliver before missing the deadline,’ Antonios says. Failure to deliver the notice within the given time frame can result in noncompliance.
While Antonios points out that CMS stated in the 2017 IPPS final rule that facilities can deliver the MOON prior to 24 hours of observation care, this may not always be the best option?especially since CMS noted that it discourages this practice. Delivering it before the 24-hour ma=rk as a proactive measure to ensure observation patients in need of the notice are not overlooked?or even delivering it on time?can present challenges since an observation stay can often become an inpatient stay based on a physician’s finding during the early hours of patient care, Antonios says.
Whether you decide to wait 24 hours or deliver the MOON as soon as observation status is initiated, there will be pros and cons.
Not waiting for the 24-hour mark may mean the verbal and written notice were given but not needed and could result in patients who are confused about their status and the financial implications of it. ‘It’s so early in the process that you may have people switched to inpatient before 24 hours and then you would have wasted the little bit of energy and resources to do a task that you didn’t need to do, because if you switch someone before 24 hours you don’t have to give them anything,’ Antonios says.
Delivering the MOON to all patients when they are first assigned to observation makes it easier to capture these Medicare beneficiaries before the 24?36-hour window passes, he says. It lends a fair amount of standardization and automation to the process of complying with the NOTICE Act and MOON, Antonios says.
However, ensuring that staff who are educated on completing the written notice and verbally explaining observation to patients are available at all times is not an easy task. While emergency departments (ED) are often well staffed during nights and weekends, other areas of hospitals may not have the same coverage, which could result in noncompliance if the MOON delivery window is missed. The ED?be it registration or other staff?may be the ideal setting for delivering the MOON if it is done routinely prior to the 24-hour mark. ‘Staffing on the floor goes down significantly after hours. It goes down significantly during the weekend, but the ED typically still has staff,’ Antonios says. ‘People receive paperwork in the ED anyway. It’s part of the process.’
HCPro.com – HIM Briefings