If you thought The Joint Commission and other accrediting organizations (AO) were already under the proverbial gun from CMS, get ready—the House Energy and Commerce committee is launching an investigation into hospital patient safety.
Laureen shows you her proprietary “Bubbling and Highlighting Technique”
Download your Free copy of my "Medical Coding From Home Ebook" at the top right corner of this page 2018 CPC Practice Exam Answer Key 150 Questions With Full Rationale (HCPCS, ICD-9-CM, ICD-10, CPT Codes) Click here for more sample CPC practice exam questions with Full Rationale Answers Click here for more sample CPC practice exam questions and answers with full rationaleTag Archives: Safety
Full Recovery Of Medical Safety Issues As “prevention”
A material display, Zhejiang has 200 children in a kindergarten there the phenomenon of abdominal lymph nodes.
Just be exposed the Acanthopanax injection to cause death, followed by anesthesia in a hospital in Fujian Province took place, “Ma” death and several incidents; the First Affiliated Hospital of Xi’an Jiaotong University for nosocomial infections caused by eight neonatal death row Event has just concluded, and now 200 “lymph child” has a collective “stage.”
The moment, there are thousands of “Stone Baby” did not discharge.
Recently be described as one trouble following another.
Objectively speaking, we do not have enough evidence to come to public health and safety incidents are more conclusive than before?? In fact, from all over the world to see, such issues have always been impressive, due to lack of information developed before or , or for information not transparent in many cases not known to the public. It should be recognized, high-speed development, we really are experiencing a high rate of public health safety frequently stage.
Sense, in social transformation, public health and safety incidents associated with certain properties. Imagine living in a blind worship of diffuse large GDP, “site” on the scene in full swing under the colors and pollution everywhere in the sharp decline in environmental quality, unless King, body, how can do it vulnerable to the attack?
From 5 years ago, “SARS” Start, health and safety incidents in recent years experienced, people can see the media an open, transparent reporting, see the Government brainer positive “response.” In this sense, the public informed of significant information in a timely, accurate, comprehensive, government departments, the emergency response of fast, efficient, can be said to the best period in history. Although these are not sufficient to eradicate hidden dangers, but expressed the government’s attitude and determination.
But no matter how good the response afterwards, some consequences are irreversible?? Mortality in the “stone” and “infected” children never grow up opportunities, died of Acanthopanax and anesthesia in patients can no longer wake up … … a heavy price in human lives to remind us that public health and safety incidents to curb the momentum of frequent, only emergency response is not enough; the work forward, firmly grasp the “prevention first” and hold the accident nipped in the bud, so no chance from the “likely” to “facts”, this is really solve the problem.
If the change concept of development, management and repair the environment, thereby reducing the food, pharmaceutical exogenous pollution, but also a very long time; then to strengthen routine health, medical supervision and law enforcement, especially against such as kindergartens, schools the hospital that some of concentrated population, prone to place health and safety incidents to increase law enforcement efforts to increase the frequency of law enforcement, it is realistic and necessary choice.
Admittedly, this operation would be difficult to be sure, at least faced the practical challenges of increased workload, the scheduling of resources will also inevitably need to make the layout again. But of greatest difficulty is not slack off even for a moment, because we can no longer try to life “poison” and rely on life alarm. If only because of the difficulties and dread not the former, then later even if there is another positive “remedial” actions, are able to escape suspicion “show” the questions and accusations.
I am an expert from China Crafts Suppliers, usually analyzes all kind of industries situation, such as felt tip pens , cd menu maker.
Related Medical Coding Articles
OIG Makes Group Home Health and Safety a Priority
By congressional request, the Office of Inspector General (OIG) prompted a series of audits, which investigated group home abuse and neglect of developmentally disabled residents. The findings were horrifying. According to their website, they “found that these residents often experienced serious injuries and medical conditions that resulted in emergency room visits,” and that “99 percent […]
AAPC Knowledge Center
Experts On The Safety Of Medical Ultrasound Domestic Issues – Ultrasound, Medical Equipment,
Institute of Acoustics, Chinese Academy of Sciences
researchers, the National Acoustic Standard Ultrasound Technology Committee – acoustic branch of the Secretary-General, Professor Niu Fengqi a recent interview, repeatedly stressed that clinicians should know about ultrasound safety regulations, knowledge and operating skills, and actively used with caution, and to prohibit application of non-medical purposes; the safety of diagnostic ultrasound is conditional, its technical progress is a benefit and Risk Coexisting double-edged sword.
Ultrasound diagnosis of the safety concept
80 years since the last century since the ultrasound was seen as a safe sound technology is widely used in China, and even become a routine pregnancy check means.
But now, the situation has changed. Bovine Fengqi told reporters, Ultrasonic wave Clinical diagnosis as information carriers must have certain safety limits in order to ensure that no parts were irradiated produce harmful biological effects. To biological effects of ultrasound on the fetus, for example, Expert Most concerned about fetal ultrasonography in the temperature, that is, the impact of thermal effects, because a large number of studies have demonstrated a teratogenic effect fever. Therefore, the focus of the study shall seek to define the possible biological effects caused by temperature and exposure time, and then determine the cause of such a temperature rise of the ultrasonic output level, and then based on these data to establish the scope or standard security applications.
Cattle Fengqi that the ultrasonic sound is nothing wrong with the early publicity, “which is based on the low output in terms of sound intensity.” Today, echocardiography (M Ultra), pulsed wave spectral Doppler, color flow imaging, the realization of many new features, often is to enhance the sound intensity for the pre-conditions and the thermal effects and mechanical effects, etc. they simply repeating what exacerbated by strong increases. The higher the sound intensity, the greater the depth imaging, image more clear, the higher signal to noise ratio when collecting information. There is no doubt enjoying the benefits of such high-tech, while the potential risk of ultrasonic irradiation is also increasing. Because of this, the international ultrasound medical sector ALARA principle of “necessary in the clinical diagnostic information can be obtained under the premise to be used at the lowest possible sound output.” This principle provides that the power output should be done with a suitable detection; If in doubt, should be low output, only when necessary, improve them; when used in obstetrics, the operating mode of each key should be placed in the lowest output adjustment state until the probe by the operator when necessary to improve the sound power.
Should keep abreast of changes in international norms
Then our clinical application of ultrasound to whether strict compliance with the relevant provisions of the security risk does not exist? Niu Fengqi not think so.
He pointed out that clinical application of color Doppler ultrasound and other high-end equipment, almost all produced in the United States and other Western countries. Published in 1985, FDA “for medical ultrasound diagnostic equipment acoustic output measurement and reporting guidelines” set forth in the body parts of the diagnostic space peak – average sound intensity (Ispta) (the most closely linked with the temperature parameters) expressed the greatest sound output: Ophthalmology , 17 mW / mm; fetus and others (including the abdomen, Pediatrics , Small parts), 94 mW / mm; heart, 430 mW / mm; peripheral, 720 mW / mm. The U.S. government in 1991 liberalized the output value of ultrasonic sound, FDA again in 1993 to achieve safe way to do Ultrasound significant changes on the one hand While the diagnosis of the biggest parts of the field restrictions remain the original value of sound intensity, but the actual product the maximum output capacity to 720 milliwatts is all relaxed / square cm; the other hand, to avoid patients suffering from high intensity irradiation of the calamity, attached prerequisites: diagnostic equipment required to install the corresponding acoustic output display system, that additional thermal index (TI ) and (or) mechanical index (MI) screen display, and provides two indices allowed limit in clinical adjustment by the operator to control the buttons on. This regulation will be greater and the ultimate responsibility to the doctor (or medical physicists), they must understand the acoustic output measurements and used to guide clinical exploration, based on differences in the clinical target selection is safe without excessive sound output level.
Ultrasound diagnostic equipment to enhance the acoustic output of the control, the International Electrotechnical Commission (IEC) in 1992 established “acoustic output of medical ultrasound diagnostic equipment disclosure requirements” (IEC61157-1992) provides the host with the probe for all the combinations work mode, the acoustic output (in water measured value), the spatial peak – average sound intensity (Ispta)
View medical device products, go to the medical device market … …
View medical device information, information into the medical device industry … …
I am an expert from replacement-projectorlamp.com, while we provides the quality product, such as Replacement Projector Lamp Manufacturer , China Bare Projector Lamps,
Find More Medical Coding Articles
CMS report focuses on AOs’ life safety short-comings
The annual CMS evaluation of accreditation organizations (AO) is out and in the hands of Congress. CMS thinks all the AOs aren’t doing as well as they should in catching violations and is promising Congress that it’s actively working to change that.
Fire doors, drills, and the ED; Joint Commission clarifies Life Safety Code requirements
In May, The Joint Commission issued clarifications on its 2012 Life Safety Code® (LSC)–related requirements for fire doors, fire drills, and emergency department (ED) occupancy. Here’s a look at the four clarifications and what they mean.
PSI 90’s transformation into the Patient Safety and Adverse Events Composite
PSI 90’s transformation into the Patient Safety and Adverse Events Composite
by Shannon Newell, RHIA, CCS, AHIMA-approved ICD-10-CM/PCS trainer
The fiscal year (FY) 2017 IPPS proposed rule alerted us to some significant changes to Patient Safety Indicator (PSI) 90, one of which is a new name: the Patient Safety and Adverse Events Composite. A fact sheet released by the measure’s owner, the Agency for Healthcare Research and Quality (AHRQ), provides insights into what may lie ahead if the proposed rule’s content is finalized.
Nothing new here
The underlying objective of this modified claims-based quality measure remains the same. The Patient Safety and Adverse Events Composite provides an overview of hospital-level quality as it relates to a set of potentially preventable hospital-related events associated with harmful outcomes for patients.
The measure will also continue to be included in CMS hospital pay-for-performance programs:
- The Hospital-Acquired Condition Reduction Program (HACRP) will adopt the measure in FY 2018
- The Hospital Value-Based Purchasing Program will adopt the measure in FY 2019 after the statutorily required one-year public posting of performance on CMS Hospital Compare under the Inpatient Quality Reporting Program
- PSI performance will still be assessed using an observed over expected ratio, and the risk adjustment methodology will remain the same, although comorbidity variables and coefficient weights will likely be refined
PSIs in the CMS composite will change
CMS has included eight PSIs in the composite used in hospital pay-for-performance programs:
- 3, pressure ulcer
- 6, iatrogenic pneumothorax
- 7, central line?associated bloodstream infection
- 8, postop hip fracture
- 12, preop pulmonary embolism or deep vein thrombosis
- 13, postop sepsis
- 14, postop wound dehiscence
- 15, accidental puncture/laceration
The modified measure will delete PSI 7 from the composite, citing duplication with other similar measures.
Three of the PSIs (8, 12, and 15) will be re-specified, which means that the types of patients included in the PSIs will be revised (see "Revised PSIs" on p. 3).
Composite weights are revised
A new algorithm that considers both the volume of events and their probability of harm will be used. The graph on p. 3 illustrates the proposed impact of each PSI’s performance on the overall composite weight. PSI 15, which at present comprises half of the composite weight, is reduced to 0.82%!
Preparation challenges
Although the HACRP will adopt this modified measure in FY 2018, performance will be based on today’s discharges. Therefore, a review of the revised measure specifications and risk adjustment variables is encouraged. The challenge: The ICD-10-ready specifications for this modified version will not be ready until sometime this summer, and the risk adjustment variables are not anticipated to be ready until next year. AHRQ is evaluating ICD-10 data in its databases to finalize this information.
What to do in the interim?
In the meantime, we recommend the following:
- Continue to use the most recent measure specifications and risk adjustment variables used by CMS for the current PSI 90 cohorts
- A close review of the ICD-10 drafts by your CDI program experts will likely identify ICD-9 to ICD-10 mappings that do not appear to support the intention of the measure
- The current ICD-10-ready drafts are just that?drafts?and AHRQ acknowledges that they will likely be refined
- Review the most recent measure specifications for the proposed new cohorts (PSI 9, 10, and 11) to identify CDI risk areas
- PSI 11, postoperative respiratory failure, has traditionally been a known CDI vulnerability
- Study the proposed re-specified measures to identify CDI opportunities
- Meet with the quality team and determine what version of measures they currently use to assess organizational performance and to get in sync on the versions impactful to CMS value-based outcomes
- Educate your CDI team and providers on PSI documentation needs, and tighten up operational processes to flag discharges that trigger the PSIs
- Don’t forget that PSI 90 is a risk-adjusted measure; the capture of comorbidities for all discharges in the measure denominators is essential to reflect accurate performance
Summary
Strong performance in patient safety events has broad implications. Patient safety events have downstream cost and quality ramifications ranging from the cost to treat the safety event to readmissions and mortality. Data quality is an essential component to appropriate focus and measurement of patient care improvement efforts.
CDI programs that have already established the infrastructure to monitor and effectively impact claims-based quality measures are likely positioned well to navigate these changing waters. Additional information can be located at www.qualityindicators.ahrq.gov/News/PSI90_Factsheet_FAQ.pdf as well as www.qualityindicators.ahrq.gov/Modules/psi_resources.aspx.
Editor’s note: Newell is the director of CDI quality initiatives for Enjoin. Her team provides health systems with physician-led education and infrastructure design to sustainably address documentation and coding challenges essential to optimal performance under value-based payments across the continuum. She has extensive operational and consulting expertise in coding and clinical documentation improvement, performance improvement, case management, and health information management. You can reach Newell at 704-931-8537 or [email protected]. Opinions expressed are that of the author and do not represent HCPro or ACDIS.
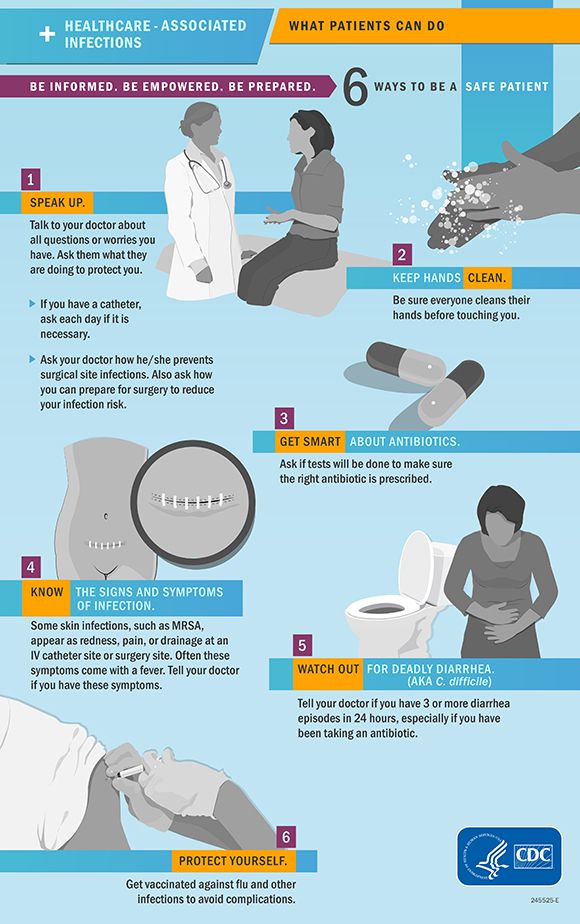
Infographic: Six Ways to Promote Patient Safety

 Minimize the Risk of Healthcare-Associated Infections
Minimize the Risk of Healthcare-Associated Infections
Healthcare-associated infections (HAI) are a significant concern for both patients and healthcare providers.
HAIs compromise patients’ treatment plans and recoveries — particularly for those who are post-op, have chronic health conditions, or compromised immune systems. HAIs, like C. diff and MRSA, are often difficult and costly to treat.
The Centers for Disease Control and Prevention (CDC) recently completed their National and State Healthcare-Associated Infections Progress Report. Here are their findings as well as six ways patients can minimize their risk of contracting HAIs.
Key Findings
One of the CDC’s goals is to implement policies and procedures that will stop the spread of HAIs. In doing so, there will be better patient outcomes and the burden on healthcare providers and facilities will be minimized.
For example, in 2011, there were approximately 722,000 HAIs in U.S. acute care hospitals, or the equivalent of 1 in 25 patients. About 75,000 patients who contracted an HAI died during their hospital stay.
The most recent report pooled 2014 national and state-level data from acute care hospitals. They evaluated the following types of infections:
- central line-associated bloodstream infections (CLABSI),
- catheter-associated urinary tract infections (CAUTI),
- surgical site infections (SSI),
- hospital-onset Clostridium difficile infections (C. difficile), and
- hospital-onset methicillin-resistant Staphylococcus aureus (MRSA) bacteremia (bloodstream infections)
On a national level, there was a decrease in the majority of infection types. Between 2008 and 2014, the rates decreased by:
- 50 percent for CLABSI
- 17 percent for abdominal hysterectomy SSI
- 2 percent for colon surgery SSI
Between 2011 and 2014, there was an 8 percent decrease in C. diff infections and a 13 percent decrease in MRSA infections.
Minimize Risks
Research has shown that healthcare facilities can minimize the occurrence of HAIs by strictly following appropriate best practices and guidelines. It’s been demonstrated that an estimated 70 percent reduction in infection rates is possible.
Additionally, patients should follow these six steps to protect against HAIs:
- Speak up. Ask your doctor or care providers how they are protecting you from infection.
- Keep hands clean. Make sure all healthcare workers cleans their hands before touching you.
- Get smart about antibiotics. Ask your doctor if testing will be done to confirm that the correct antibiotic is prescribed.
- Know the signs and symptoms of infection. Infections present differently – know the signs and symptoms of the most common ones.
- Watch out for deadly diarrhea. Report any ongoing episodes of diarrhea to your physician.
- Protect yourself. Avoid complications by opting to receive vaccinations for potentially life-threatening infections.
To see each state’s infection rates, check out the full CDC report. The CDC also released a handy infographic about preventing the spread of HAIs. You can find that below.
How did your state rate? What steps do you take to prevent HAIs? Please tell me in the comments below!
This post Infographic: Six Ways to Promote Patient Safety was written by Manny Oliverez and first appeared on Capture Billing. Capture Billing is a medical billing company helping medical practices get their insurance claims paid faster, easier and with less stress allowing doctors to focus on their patients.






