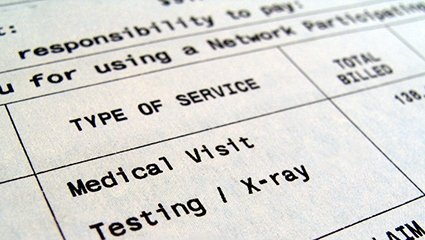
Recently there has been a lot of discussion in the self-funded world about Reference-Based Pricing (RBP) and the vendors offering this solution to help these plans save money. The model used in this context advertises an "open network" (go to any provider) then provides the employer with a medicare-based (or cost-based) cap on the payment for services and legal defense for employees who are balance billed. I’ve seen a few law suits pop up this year regarding this model (Utah and California) and there is ample online documentation on the payor side on how to implement (with language templates), but there doesn’t appear to be much in the public domain (on the provider side) identifying a clear process on how this sort of plan is handled in the revenue cycle. Is anybody aware of posted statement, template letter responses, seminars from conferences, or powerpoints put together by contracting/collection vendors for providers that explains how to address self-funded Reference-Based Pricing plans. I am asking because I would like to write an article about how reference-based pricing has increased in self-funding, and how providers have responded. For the moment, the general vendor sales documents online say that most providers accept these rates and very few providers balance bill the patients. I’ve even read the slogan "The best way to pay less for healthcare, is to pay less for healthcare." The few lawsuits I have found seem to indicate some systems do not accept this payor model, but outside of a letter or two I have yet to find any primary sources identifying a comprehensive approach or hospital system posted statements that this type of insurance is not accepted. I’d really appreciate some facility posted statements or collection vendor template documents that would allow the article to present the entire present picture for this RBP movement in the self-funded world.
Medical Billing and Coding Forum