Reimbursement Information:
Reimbursement for allergy testing services includes the following components,
- Supplies (e.g., sterile diluents, syringes, needles)
- Monitoring the physical status of the patient during testing
- Observation, recording, and interpretation of the test results
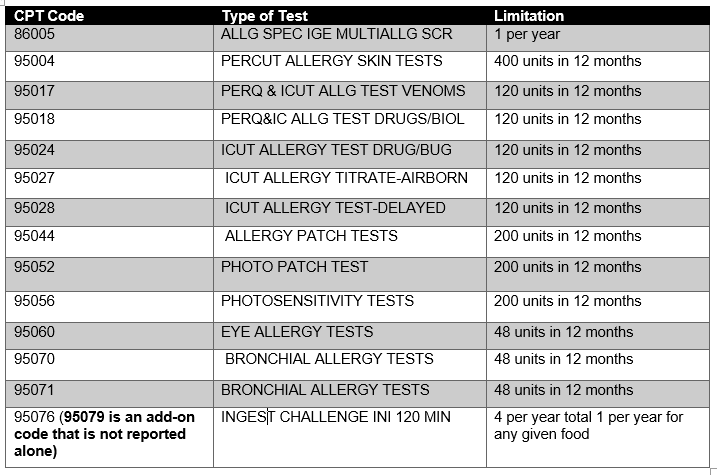
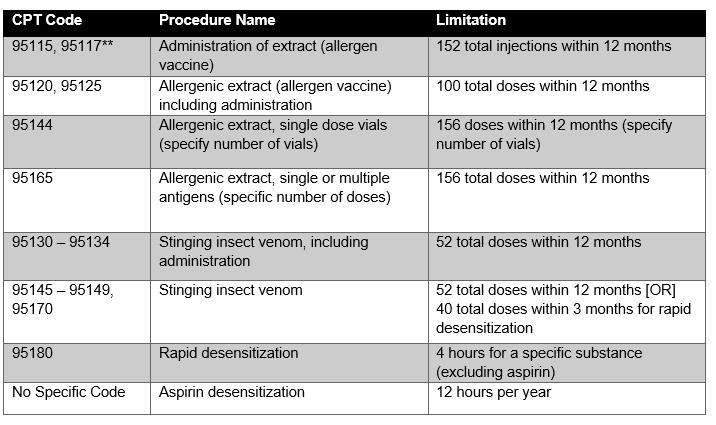
Reimbursement for “allergy testing” is based on the number of each type of test performed by the same physician and is subject to the following limitations when the above coverage criteria are met,